Neurology Report
Auckland
District Health Board
Auckland Hospital
Park Road
Private Bag 92-024,
Auckland 1,
New Zealand
Telephone: 0-9-379-7440
Service: Neurology Department
Phone: 09-307-4949
Ext: x 25823
Fax: 09-375-4309 or 5209 internal
11 February 2008
TO WHOM IT MAY CONCERN
Re: Wayne Michael DOUGLAS, dob : 9-9-66
NHI : PJU6268
I have been a Consultant Neurologist for 15 years. I received neurological training in Auckland, New Zealand, and at the Mayo Clinic, Rochester, Minnesota, USA. I have been working full-time as a Consultant Neurologist at Auckland City Hospital since 1995.
I have seen Wayne Douglas on two occasions at Auckland City Hospital: on 12 December 2001 and on 1 October 2003.
Mr Douglas has told me that one day in May 2000 he woke during the night with intense vertigo and unsteadiness on his feet. The vertigo had partially resolved after eight hours but he remained unable to walk without support for a week. He was seen urgently at the STRC Hospital where an MRI scan of the brain was negative. His symptoms were thought to be due to Vestibular Neuronitis and he was prescribed several medications which he took for one month. For 2.5 years following this he had a fluctuating, low-grade sensation of imbalance in his head.
In June 2000 Mr Douglas consulted Dr X. Dr X apparently told Mr Douglas that he had Sylvian Aquaduct Syndrome. He was prescribed five different medications to be taken concurrently. Mr Douglas then developed a wide range of additional symptoms, some or all consistent with exposure to benzodiazepine medications.
Neurologic examinations by me in 2001 and 2003 have not shown any residual neurological signs.
I would agree with doctors at the STRC Hospital that Mr Douglas most likely had an episode of Acute Vestibulopathy in May 2000. This condition has multiple synonyms including Vestibular Neuronitis, Acute Vestibular Neuritis, Acute Labyrinthitis and Neurolabyrinthitis. The preferred expression is Acute Unilateral Peripheral Vestibulopathy (1). It refers to an acute lesion of the vestibular apparatus (semicircular canals and related structures) or vestibular nerve on one or other side. Most clinical neurologists will encounter one or more cases each year, although the patient is sometimes not seen until after the acute symptoms have resolved. The clinical features include intense vertigo, vomiting, and unsteadiness of gait. Neurologic examination in the acute phase shows unidirectional nystagmus with the fast phase away from the affected ear(2). Some authorities believe that Acute Unilateral Peripheral Vestibulopathy is due to reactivation of Herpes Simplex virus infection (3). The patient’s symptoms usually subside gradually over days to weeks.
A range of neurological conditions (for example, cerebellar infarction, multiple sclerosis) can mimic Acute Unilateral Peripheral Vestibulopathy, but all are excluded or made very unlikely if the brain MRI scan is negative. Methylprednisolone significantly improves the recovery of peripheral vestibular function in patients with Acute Unilateral Peripheral Vestibulopathy (3). Patients are sometimes also administered intravenous fluids and anti-emetics.
The Sylvian Aqueduct Syndrome is rare and seldom encountered in modern neurological practice. A literature search in February 2008 (Pubmed) using the expression “Sylvian Aqueduct Syndrome” yielded just 23 articles since 1966, with only 3 articles in the past 20 years. It refers to a syndrome whose features include vertical gaze restriction, abnormal pupillary reaction, upper lid retraction, and convergence–retraction eye movements. Paralysis of convergence and skew deviation may also occur. Sylvian aqueduct syndrome usually occurs in patients with shunted hydrocephalus whose shunts become blocked (4). Single case reports have also described the syndrome in patients with midbrain infarction (5), multiple sclerosis (6), thalamic haemorrhage (7), tumours in the pineal region (8) and unilateral midbrain lesions (9). Mr Douglas apparently did not have the above constellation of neurological signs, but more importantly his brain MRI scan did not show hydrocephalus or any other disorder which can produce the Sylvian Aqueduct Syndrome.
I do not know of any reason, theoretical or otherwise, why benzodiazepine medication would have had a role in the treatment of Mr Douglas in 2000. Benzodiazepine drugs do not have useful anti-emetic or anti-vertiginous properties and have no clear role in the treatment of Acute Unilateral Peripheral Vestibulopathy. Further, benzodiazepine drugs would not be effective in treating hydrocephalus or any of the other conditions which may produce the Sylvian Aqueduct Syndrome.
REFERENCES
1. In: Baloh RW, Halmagyi GM, eds. Disorders of the vestibular system. New York: Oxford University Press, 1996:318–27.]
2. Halmagyi GM, Cremer PD. Assessment and treatment of dizziness. J Neurol Neurosurg Psychiatry. 2000 Nov;69(5):706.
3. M Strupp, V Zingler, V Arbusow, et al. Methylprednisolone, Valacyclovir, or the Combination for Vestibular Neuritis. N Engl J Med 2004;351:354-61
4. J Neurosurg. 1999 Jul;91(1):169-70.
5. Hommel M, Besson G. Midbrain infarcts. In: Bogousslavsky J, Caplan LR, editors. Stroke syndromes. New York: Cambridge University Press, 1995:336-43
6. Koshimura I, Nishi K, Komiya T, Mizuno Y. Pretectal syndrome caused by a plaque of multiple sclerosis. Rinsho Shinkeigaku. 1994 Mar;34(3):236-40.
7. Shigemori M, Shirahama M, Hara K, Tokutomi T, Kojima Y. A case of sylvian aqueduct syndrome secondary to thalamic hemorrhage. Rinsho Shinkeigaku. 1981 Aug;21(8):721-7.
8. Sakata E, Nakaigawa K, Itoh Y, Takahashi K. Sylvian aqueduct syndrome. Chronology of tumors in the pineal region in view of ocular movement. Auris Nasus Larynx. 1984;11(2):101-8.
9. Auerbach SH, De Piero TJ, Romanul F. Sylvian aqueduct syndrome caused by unilateral midbrain lesion. Ann Neurol. 1982 Jan;11(1):91-4
David Hutchinson
MB ChB FRACP
Neurologist
Top of Page
The primary language of this website is English. Japanese appears as translations only (except for some original court documents).
These translations have been done by many different translators including me. Therefore, there are differences in quality and styles.
Please understand that I am not native Japanese and subsequently there are parts that may sound unnatural in Japanese.
“If any drug over time is going to just rob you of your identity [leading to] long, long term disaster, it has to be benzodiazepines.”
Dr John Marsden,
Institute of Psychiatry, London
November 1, 2007
“Benzos are responsible for more pain, unhappiness and damage than anything else in our society.”
Phil Woolas MP,
Deputy Leader of the House of Commons,
Oldham Chronicle, February 12, 2004
“It is more difficult to withdraw people from benzodiazepines than it is from heroin.”
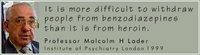
Professor Malcolm H Lader
Institute of Psychiatry London
BBC Radio 4, Face The Facts
March 16, 1999