CHAPTER I (PART 1)
THE BENZODIAZEPINES: WHAT THEY DO IN THE BODY
CHAPTER ONE (PART 1) CONTENTS
- Potency
- Speed of elimination
- Duration of effects
- Therapeutic actions of benzodiazepines
- Mechanisms of action
Table 1. Benzodiazepines and similar drugs
Table 2. Therapeutic actions of benzodiazepines
Fig. 1. Diagram of mechanism of action of the natural neurotransmitter GABA (gamma aminobutyric acid) and benzodiazepine on nerve cells (neurons) in the brain
Top of Page
BACKGROUND
For twelve years (1982-1994) I ran a Benzodiazepine Withdrawal Clinic for people wanting to come off their tranquillisers and sleeping pills. Much of what I know about this subject was taught to me by those brave and long-suffering men and women. By listening to the histories of over 300 "patients" and by closely following their progress (week-by-week and sometimes day-by-day), I gradually learned what long-term benzodiazepine use and subsequent withdrawal entails.
Most of the people attending the clinic had been taking benzodiazepines prescribed by their doctors for many years, sometimes over 20 years. They wished to stop because they did not feel well. They realised that the drugs, though effective when first prescribed, might now be actually making them feel ill. They had many symptoms, both physical and mental. Some were depressed and/or anxious; some had "irritable bowel", cardiac or neurological complaints. Many had undergone hospital investigations with full gastrointestinal, cardiological and neurological screens (nearly always with negative results). A number had been told (wrongly) that they had multiple sclerosis. Several had lost their jobs through recurrent illnesses.
The experiences of these patients have since been confirmed in many studies, by thousands of patients attending tranquilliser support groups in the UK and other parts of Europe, and by individuals vainly seeking help in the US. It is interesting that the patients themselves, and not the medical profession, were the first to realise that long-term use of benzodiazepines can cause problems.
Top of Page
ABOUT THIS CHAPTER
Some readers may decide to go directly to the chapter on benzodiazepine withdrawal (Chapter II). However, those who wish to understand withdrawal symptoms and techniques (and therefore to cope better with the withdrawal process) are advised to become acquainted first with what benzodiazepines do in the body, how they work, how the body adjusts to chronic use, and why withdrawal symptoms occur. These issues are discussed in this chapter.
Top of Page
THE BENZODIAZEPINES
Potency
A large number of benzodiazepines are available (Table 1). There are major differences in potency between different benzodiazepines, so that equivalent doses vary as much as 20-fold. For example, 0.5 milligrams (mg) of alprazolam (Xanax) is approximately equivalent to 10mg of diazepam (Valium). Thus a person on 6mg of alprazolam daily, a dose not uncommonly prescribed in the US, is taking the equivalent of about 120mg of diazepam, a very high dose. These differences in strength have not always been fully appreciated by doctors, and some would not agree with the equivalents given here. Nevertheless, people on potent benzodiazepines such as alprazolam, lorazepam (Ativan) or clonazepam (Klonopin) tend to be using relatively large doses. This difference in potency is important when switching from one benzodiazepine to another, for example changing to diazepam during the withdrawal, as described in the next chapter.
Top of Page
Speed of elimination
Benzodiazepines also differ markedly in the speed at which they are metabolised (in the liver) and eliminated from the body (in the urine) (Table 1). For example, the "half-life" (time taken for the blood concentration to fall to half its initial value after a single dose) for triazolam (Halcion) is only 2-5 hours, while the half-life of diazepam is 20-100 hours, and that of an active metabolite of diazepam (desmethyldiazepam) is 36-200 hours. This means that half the active products of diazepam are still in the bloodstream up to 200 hours after a single dose. Clearly, with repeated daily dosing accumulation occurs and high concentrations can build up in the body (mainly in fatty tissues). As Table 1 shows, there is a considerable variation between individuals in the rate at which they metabolise benzodiazepines.
Table 1. Benzodiazepines and Similar Drugs5
|
|
[active metabolite] |
|
Oral dosages (mg)3 |
| Alprazolam (Xanax) |
|
|
|
| Bromazepam (Lexotan, Lexomil) |
|
|
|
| Chlordiazepoxide (Librium) |
|
|
|
| Clobazam (Frisium) |
|
|
|
| Clonazepam (Klonopin, Rivotril) |
|
|
|
| Clorazepate (Tranxene) |
|
|
|
| Diazepam (Valium) |
|
|
|
| Estazolam (ProSom) |
|
|
|
| Flunitrazepam (Rohypnol) |
|
|
|
| Flurazepam (Dalmane) |
|
|
|
| Halazepam (Paxipam) |
|
|
|
| Ketazolam (Anxon) |
|
|
|
| Loprazolam (Dormonoct) |
|
|
|
| Lorazepam (Ativan) |
|
|
|
| Lormetazepam (Noctamid) |
|
|
|
| Medazepam (Nobrium) |
|
|
|
| Nitrazepam (Mogadon) |
|
|
|
| Nordazepam (Nordaz, Calmday) |
|
|
|
| Oxazepam (Serax, Serenid, Serepax) |
|
|
|
| Prazepam (Centrax) |
|
|
|
| Quazepam (Doral) |
|
|
|
| Temazepam (Restoril, Normison, Euhypnos) |
|
|
|
| Triazolam (Halcion) |
|
|
|
| Non-benzodiazepines with similar effects4,5 |
|
|
|
| Zaleplon (Sonata) |
|
|
|
| Zolpidem (Ambien, Stilnoct) |
|
|
|
| Zopiclone (Zimovane, Imovane) |
|
|
|
| Eszopiclone (Lunesta) |
|
|
|
-
Half-life: time taken for blood concentration to fall to half its peak value after a single dose. Half-life of active metabolite shown in square brackets. This time may vary considerably between individuals.
-
Market aim: although all benzodiazepines have similar actions, they are usually marketed as anxiolytics (a), hypnotics (h) or anticonvulsants (e).
-
These equivalents do not agree with those used by some authors. They are firmly based on clinical experience but may vary between individuals.
-
These drugs are chemically different from benzodiazepines but have the same effects on the body and act by the same mechanisms.
-
All these drugs are recommended for short-term use only (2-4 weeks maximum).
Top of Page
Duration of effects
The speed of elimination of a benzodiazepine is obviously important in determining the duration of its effects. However, the duration of apparent action is usually considerably less than the half-life. With most benzodiazepines, noticeable effects usually wear off within a few hours. Nevertheless the drugs, as long as they are present, continue to exert subtle effects within the body. These effects may become apparent during continued use or may appear as withdrawal symptoms when dosage is reduced or the drug is stopped.
Top of Page
Therapeutic actions of benzodiazepines
Regardless of their potency, speed of elimination or duration of effects, the actions in the body are virtually the same for all benzodiazepines. This is true whether they are marketed as anxiolytics, hypnotics or anti-convulsants (Table 1). All benzodiazepines exert five major effects which are used therapeutically: anxiolytic, hypnotic, muscle relaxant, anticonvulsant and amnesic (impairment of memory) (Table 2).
Table 2. Therapeutic Actions of Benzodiazepines
(In Short-Term Use)
| Action |
|
|
| Anxiolytic | - relief of anxiety | - Anxiety and panic disorders, phobias |
| Hypnotic | - promotion of sleep | - Insomnia |
| Myorelaxant | - muscle relaxation | - Muscle spasms, spastic disorders |
| Anticonvulsant | - stop fits, convulsions | - Fits due to drug poisoning, some forms of epilepsy |
| Amnesia | - impair short-term memory | - Premedication for operations, sedation for minor surgical procedures |
Other clinical uses, utilising combined effects:
- Alcohol detoxification
- Acute psychosis with hyperexcitability and aggressiveness
These actions, exerted by different benzodiazepines in slightly varying degrees, confer on the drugs some useful medicinal properties. Few drugs can compete with them in efficacy, rapid onset of action and low acute toxicity. In short-term use, benzodiazepines can be valuable, sometimes even life-saving, across a wide range of clinical conditions as shown in Table 2. Nearly all the disadvantages of benzodiazepines result from long-term use (regular use for more than a few weeks). The UK Committee on Safety of Medicines in 1988 recommended that benzodiazepines should in general be reserved for short-term use (2-4 weeks only).
Top of Page
Mechanisms of action
Anyone struggling to get off their benzodiazepines will be aware that the drugs have profound effects on the mind and body apart from the therapeutic actions. Directly or indirectly, benzodiazepines in fact influence almost every aspect of brain function. For those interested to know how and why, a short explanation follows of the mechanisms through which benzodiazepines are able to exert such widespread effects.
All benzodiazepines act by enhancing the actions of a natural brain chemical, GABA (gamma-aminobutyric acid). GABA is a neurotransmitter, an agent which transmits messages from one brain cell (neuron) to another. The message that GABA transmits is an inhibitory one: it tells the neurons that it contacts to slow down or stop firing. Since about 40% of the millions of neurons all over the brain respond to GABA, this means that GABA has a general quietening influence on the brain: it is in some ways the body's natural hypnotic and tranquilliser. This natural action of GABA is augmented by benzodiazepines which thus exert an extra (often excessive) inhibitory influence on neurons (Fig. 1).
Fig. 1. Diagram of mechanism of action of the natural neurotransmitter GABA
(gamma-aminobutyric acid) and benzodiazepines on nerve cells (neurons) in the brain
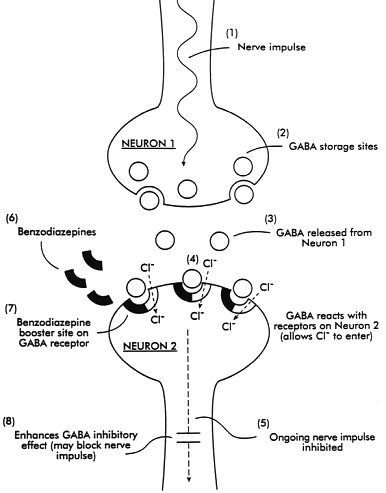
| (1,2) | Nerve impulse causes release of GABA from storage sites on neuron 1 |
| (3) | GABA released into space between neurons |
| (4) | GABA reacts with receptors on neuron 2; the reaction allows chloride ions (Cl-) to enter the neuron |
| (5) | This effect inhibits further progress of the nerve impulse |
| (6,7) | Benzodiazepines react with booster site on GABA receptors |
| (8) | This action enhances the inhibitory effects of GABA; the ongoing nerve impulse may be completely blocked |
The way in which GABA sends its inhibitory message is by a clever electronic device. Its reaction with special sites (GABA-receptors) on the outside of the receiving neuron opens a channel, allowing negatively charged particles (chloride ions) to pass to the inside of the neuron. These negative ions "supercharge" the neuron making it less responsive to other neurotransmitters which would normally excite it. Benzodiazepines also react at their own special sites (benzodiazepine receptors), situated actually on the GABA-receptor. Combination of a benzodiazepine at this site acts as a booster to the actions of GABA, allowing more chloride ions to enter the neuron, making it even more resistant to excitation. Various subtypes of benzodiazepine receptors have slightly different actions. One subtype (alpha 1) is responsible for sedative effects, another (alpha 2) for anti-anxiety effects, and both alpha 1 and alpha 2, as well as alpha 5, for anticonvulsant effects. All benzodiazepines combine, to a greater or lesser extent, with all these subtypes and all enhance GABA activity in the brain.
As a consequence of the enhancement of GABA's inhibitory activity caused by benzodiazepines, the brain's output of excitatory neurotransmitters, including norepinephrine (noradrenaline), serotonin, acetyl choline and dopamine, is reduced. Such excitatory neurotransmitters are necessary for normal alertness, memory, muscle tone and co-ordination, emotional responses, endocrine gland secretions, heart rate and blood pressure control and a host of other functions, all of which may be impaired by benzodiazepines. Other benzodiazepine receptors, not linked to GABA, are present in the kidney, colon, blood cells and adrenal cortex and these may also be affected by some benzodiazepines. These direct and indirect actions are responsible for the well-known adverse effects of dosage with benzodiazepines.
Top of Page